A Patient-Friendly Guide to Understanding Third Molar Extraction
2025-02-15
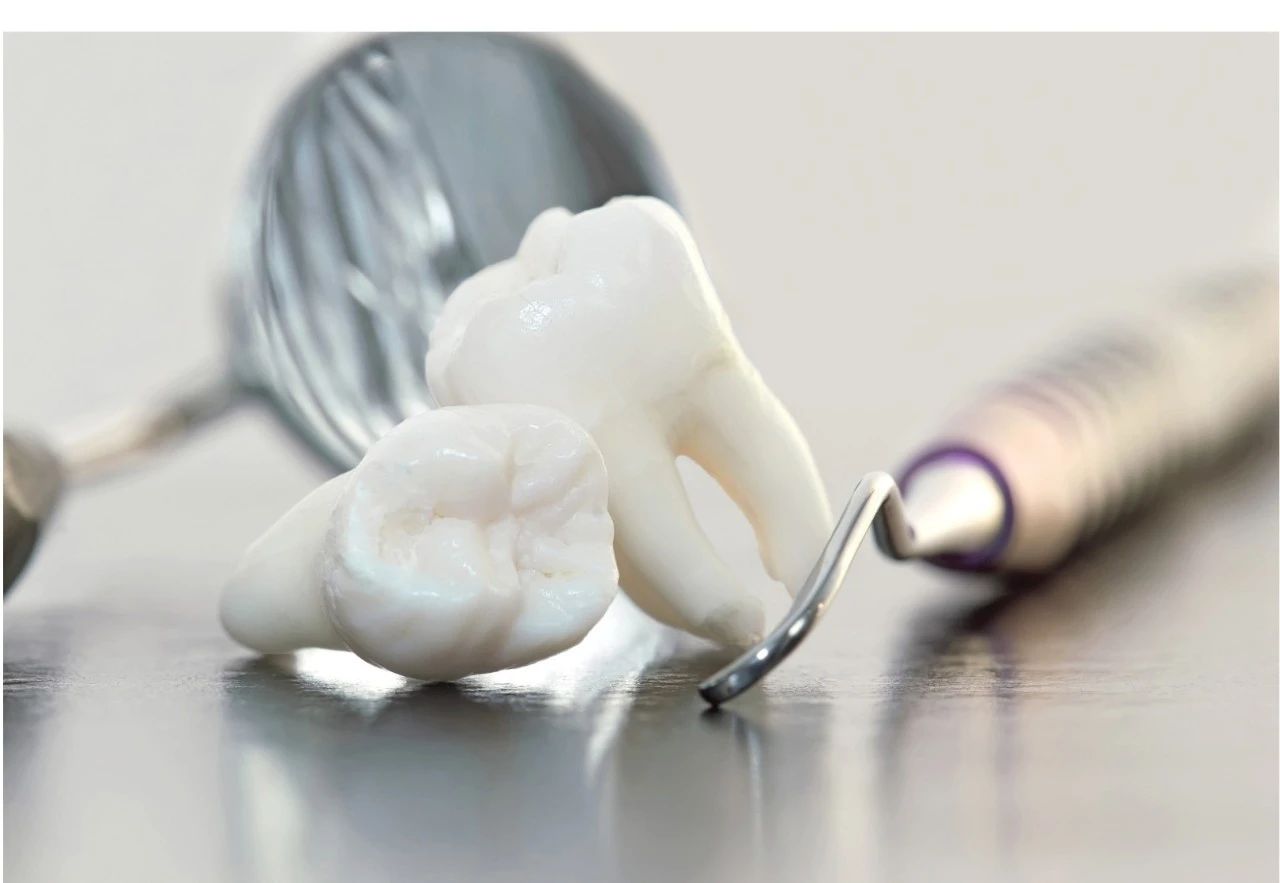
Extraction of third molars, commonly known as wisdom teeth, is a common dental procedure performed to alleviate various dental issues and is one of the most common oral surgeries performed worldwide. While the thought of undergoing a tooth extraction evokes anxiety in many individuals, understanding the procedure and recovery process can help ease concerns. In this article, we will provide a patient-friendly explanation of the extraction procedure, its benefits, and the expected recovery time. 1. What Are Third Molars?
Third molars are the last teeth to emerge, usually between the ages of 17 and 25. While some individuals have sufficient space in their jaws for these teeth to erupt properly, many experience issues due to limited room or misalignment.
Common complications involving third molars include:
Impaction: When the tooth is trapped under the gum or jawbone.
Crowding: Disruption of neighboring teeth’s alignment.
Infections: Partial eruption creates pockets for bacteria.
For patients, these complications can lead to pain, swelling, or difficulty cleaning the area.
2. Why Are Third Molars Removed?
Extraction is often recommended to prevent or address specific dental problems:
Impaction-Related Issues: Pain, swelling, or cyst formation due to trapped teeth.
Damage to Nearby Teeth: Pressure from wisdom teeth can erode adjacent molars.
Orthodontic Concerns: Wisdom teeth may interfere with teeth alignment post-braces.
Infections: Partially erupted wisdom teeth can lead to pericoronitis (gum infection).
Preventative Care: In some cases, removal is advised to prevent future complications.
3. Preparing for the Procedure:
Patients often wonder if extraction is necessary. For clinicians, the decision is based on thorough examination and assessment of symptoms.
Consultation: A dentist or oral surgeon will examine your teeth and review imaging. Use of panoramic X-rays or CBCT scans is common to evaluate tooth position and proximity to structures like the mandibular nerve or maxillary sinus. Your surgeon will use this data to plan for incision design, bone removal, and extraction technique to minimize trauma and will clearly explain the procedure and post-op care to alleviate patient concerns.
Anesthesia Options: Discuss with your surgeon whether local anesthesia, sedation, or general anesthesia is right for you.
Medical History: Share any chronic conditions, medications, or allergies.
4. The Extraction Procedure
The extraction of third molars should be performed by a qualified oral surgeon or dentist in a dental office or outpatient surgical center.
Based on the assessment, the extraction procedure may vary:
Simple Extraction: If the wisdom tooth has fully erupted and is easily accessible, a simple extraction may be performed. In this case, the oral surgeon or dentist will gently loosen the tooth using specialized dental instruments and remove it from the socket.
Surgical Extraction: If the wisdom tooth is impacted (partially or fully submerged beneath the gum line) or positioned in an awkward angle, a surgical extraction may be necessary.
Whether simple or surgical, wisdom tooth removal involves these steps:
1.Anesthesia Administration:
Local anesthesia numbs the area. Sedation or general anesthesia may be used for more complex cases or anxious patients.
2.Tooth Removal:
The surgeon will make an incision, remove bone if needed, and extract the tooth in whole or sections.Techniques vary based on the tooth’s position. For impacted teeth, sectioning the tooth reduces stress on the surrounding structures.
3.Closure and Hemostasis:
Sutures will be placed to aid healing and initially gauze is used to control bleeding.
During the extraction process, patients may experience slight pressure or discomfort, but they should not feel any pain due to the anesthesia. The duration of the procedure varies depending on the complexity of the case but typically ranges from 20 minutes to an hour.
5. Recovery Guidelines
Following the extraction procedure, patients are provided with post-operative instructions to promote healing and minimize discomfort. These instructions may include:
Applying ice packs to the affected area to reduce swelling.
Taking prescribed pain medication as directed to manage discomfort.
Eating soft foods and avoiding hard or crunchy foods that may irritate the extraction site.
Avoiding vigorous rinsing or spitting to prevent dislodging the blood clot, which is essential for proper healing.
Maintaining proper oral hygiene by gently brushing and flossing the teeth, avoiding the extraction site.
The initial recovery period after wisdom tooth extraction typically lasts for a few days to a week. During this time, patients may experience some common symptoms, including swelling, mild bleeding, discomfort, and stiffness of the jaw. These symptoms gradually subside as the extraction site heals.
It is essential for patients to follow up with their oral surgeon or dentist for a post-operative evaluation to ensure proper healing and address any concerns or complications that may arise.
6. Signs of Post Operative Complications
Patients should watch for:
Severe pain beyond the first few days.
Persistent swelling or fever (potential infection).
Unusual sensations like tingling, which may indicate nerve involvement.
Your surgeon and nursing team will keep in touch with you after the surgery because promptly managing complications like dry socket or infection is essential.
Conclusion:
Extraction of third molars, or wisdom teeth, is a common dental procedure aimed at alleviating various dental issues. By understanding the procedure and recovery process, patients can approach the extraction with confidence and peace of mind. If you are considering wisdom tooth extraction or have been recommended for the procedure, it is essential to consult with a qualified oral surgeon or dentist to discuss your specific case and address any concerns you may have.
Article contributed by Dr. Nikola Urosevic, Dentist of Parkway.